The ketogenic diet is of great interest to people suffering from autoimmune diseases such as psoriasis. This curiosity seems to come mainly from anecdotes appearing on social media. Currently available scientific evidence for the effectiveness of the ketogenic diet in psoriasis is extremely limited. However, this does not mean that this diet does not make sense – it is simply too early to make a final verdict for or against its use. Considering the amount of anecdotal evidence, it is worth analyzing how the ketogenic diet could reduce the symptoms of psoriasis and whether it is worth experimenting with and safe.
How does the ketogenic diet work?
Our daily diet consists of three groups of macronutrients: carbohydrates, proteins and fats. A standard diet provides 45-65% calories from carbohydrates, 20-35% from fats, and 10-35% from proteins. The energy we burn during our daily activities comes primarily from glucose (obtained from carbohydrates) through a process called glycolysis.
The ketogenic diet completely reverses the macronutrient ratios – fat intake is increased to 70% of daily calories, carbohydrates are reduced to only 10%, and protein takes up the remaining 20% of the diet. Such a small amount of carbohydrates is not enough to provide the energy needed to survive. For this reason, our body must activate a cascade of metabolic changes in order to provide alternative energy sources.
Once glucose stores run out, fatty acids will have to become the main source of energy – both those supplied with the diet and those accumulated in the adipose tissue. Small amounts of glucose can be made in the liver (from lactate, amino acids and glycerol) during a process called gluconeogenesis. Liver also plays the main role in the process, from which the ketogenic diet gets its name: ketogenesis. In this process, ketone bodies are formed: beta-hydroxybutyric acid, acetoacetic acid and acetone. Many organs in the human body can use ketone bodies as an alternative energy source if glucose is lacking.
It is worth noting that ketogenesis is triggered when insulin levels are very low. This is what happens when we are on a low-carbohydrate diet, when we don’t eat for an extended period of time, but also when our body doesn’t produce insulin as a result of an illness. For this reason, ketone bodies can also be produced in diabetic patients if a sudden and severe drop in insulin occurs (e.g. as a result of discontinuation of insulin therapy). Excessive production of ketone bodies can lead to the development of ketoacidosis – one of the most dangerous complications of diabetes. The risk of ketoacidosis is low in healthy people following a ketogenic diet. However, there are some exceptions (1,2,3).
Ketogenic diet and psoriasis
Can the mechanism behind the ketogenic diet be applied to the treatment of psoriasis? Yes, but also no. Let’s look at the four aspects of the ketogenic diet that are most likely responsible for its popularity.
Gut microbiome and immune response
The gut microbiome plays a key role in the physiology of psoriasis. A ketogenic diet can significantly affect the functioning of intestinal microbes in two ways.
Firstly, the ketone bodies themselves can alter the composition of the microbiome. A study published in 2020 in the prestigious scientific journal Cell found that beta-hydroxybutyrate (one of the ketone bodies) can decrease the population of the Bifidobacterium bacteria in mice (4). Meanwhile, there is evidence pointing to the anti-inflammatory and immunomodulatory effects of this bacteria species, which is why we often find it in probiotic supplements (5, 6).
The problem with the gut microbiome research is that we still don’t really know what a healthy gut microbiome is. Moreover, we don’t understand many interactions that take place between the microorganisms in our intestines. In the aforementioned article, although a decrease in the number of Bifidobacterium bacteria was observed, a reduction in intestinal inflammation was also reported. The anti-inflammatory effect occurred through inhibition of Th17 cells – hallmark inflammatory pathway in psoriasis (7).
Moreover, it has also been shown that sodium butyrate (a close relative of beta-hydroxybutyrate) also leads to a significant decrease in the number of Bifidobacterium (4). Butyrate is a product of bacterial fermentation in the large intestine and is an extremely important source of energy for the intestinal epithelial cells. Butyrate has a well-proven anti-inflammatory effect in the gut, but also via the skin-gut axis and directly on the inflammatory pathway that underpins the pathogenesis of psoriasis (8). Therefore, butyrate exhibits therapeutic potential, despite blocking bacteria commonly regarded as probiotic. Perhaps modulating the microbiome to reduce the number of Bifidobacterium in certain cases is not only harmless but also desirable. For now, we can only speculate.
Secondly, ketogenic diet is often low in fiber due to the elimination of (whole) grains, fruits and many vegetables. Of course, ketogenic diet doesn’t have to be fiber-deficient. However, getting enough fiber is not easy and requires quite a bit of planning. While we don’t know much about the composition of a healthy microbiome, we do know for certain that fiber is key to maintaining gut health (9). Therefore, it is not surprising that studies looking at the gut microbiome during ketogenic diet point to a reduction in the diversity of microorganisms inhabiting the intestines. Moreover, reduction in the number of health-promoting bacteria (including Bifidobacterium) and an increase in the number of pathogenic bacteria, such as E. coli has also been observed during ketogenic diet (10, 11). Therefore, the low-fiber ketogenic diet has the potential to negatively impact gut health, which is already weakened in psoriasis patients. Find out more about increased intestinal permeability in psoriasis here.
Weight-loss
In the case of overweight or obese people, reducing body fat leads to a significant reduction in the intensity of psoriasis symptoms (12). The ketogenic diet is very effective when it comes to reducing body fat. Many people experience weight loss after switching to the ketogenic diet, even if caloric restriction was not intentional.
This is mainly due to increased insulin sensitivity and decreased appetite. What’s more, the very fast pace of weight loss (including significant water-loss) motivates people who want to get rid of excess body fat to continue adhering to the diet. And of course – the most effective diet is the one that you actually follow.
Several studies have tested an extremely aggressive way of losing weight via a very low-calorie ketogenic diet in people with psoriasis (13, 14, 15). These studies showed promising results, but it is worth remembering that any diet will lead to a reduction in body fat as long as the caloric expenditure is greater than the amount of calories consumed. Therefore, the fact that a low-calorie ketogenic diet is effective in the treatment of psoriasis is not an argument in favor of a ketogenic diet, but in favor of a calorie-deficient diet.
I suspect that some of the positive effects commonly attributed to the ketogenic diet are simply due to deliberate or accidental reduction in body fat. These effects are real, but they could as well be achieved through a less restrictive diet. It is also worth noting that the greatest difficulty in losing weight is not losing body fat but maintaining a healthy weight after completing the diet. Consider what will happen once you reach your target weight – if you go back to your usual diet, there is a high risk that the kilograms will come back as well. For this reason, it is worth choosing less drastic solutions, focused on long-term effects rather than shock-therapy.
Accidental elimination of nutritional triggers
Another phenomenon that may explain the popularity of the ketogenic diet is the accidental elimination of nutritional triggers of the disease. People with psoriasis often suffer from food intolerances. The most common triggers include certain grains, fruits and vegetables – all significant sources of carbohydrates, eliminated during the ketogenic diet. Moreover, this diet also excludes many highly processed foods (e.g. sweets) containing food additives, which may also aggravate the symptoms of psoriasis in some patients. Food intolerances are not always correctly identified. So perhaps the positive effects of the ketogenic diet come from the the accidental exclusion of triggering foods, not the ketosis itself. It’s worth noting that the ketogenic diet is also a gluten-free diet. Gluten is one of the best-studied triggers of psoriasis, you can find a blog post on this topic here.
Placebo effect
The power of the placebo effect is often underestimated. Here I would like to introduce you to my favorite study on this subject, titled Mind over milkshakes (16).
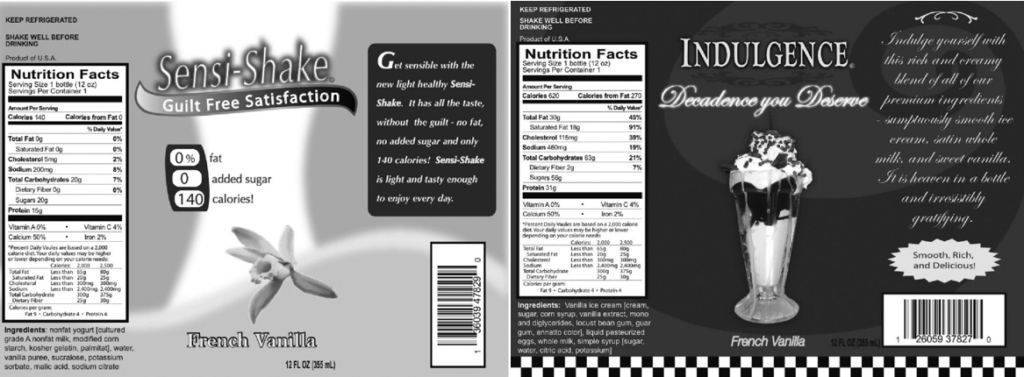
During this study, participants received two milkshakes, both with an average caloric value (380 kcl). During the first session, the milkshake was presented as high-calorie, high-fat and indulgent. After a week, the participants took part in the second session, during which the same milkshake was presented as a 'diet’ product, i.e. low-calorie and low-fat. Both versions of the milkshake had fake labels, which you can find below. Besides the label, both milkshakes remained exactly the same.
Ghrelin (the hormone responsible for feeling hungry) was measured before, during and after consuming the milkshakes. When participants consumed the milkshake described as low-calorie, their ghrelin levels increased slightly – as if they were actually consuming a small number of calories. However, after consuming the milkshake described as high in calories, ghrelin increased to a high level – as if the participants had consumed a truly high-calorie product.
The results of this study show us that mindsets can dictate the physiological responses of our body. Perhaps the phenomenon of the ketogenic diet is at least partly the result of an extremely strong belief that this diet will be beneficial. This does not mean that the effects seen by people following this diet are „in their heads”. These effects are real, but their nature may be different than it seems at first glance …
To sum up
Currently, we don’t have enough scientific evidence to recommend the ketogenic diet to psoriasis patients. Moreover, we don’t know what happens when the ketogenic diet is used long-term. Considering the above-mentioned cases of ketoacidosis, the risk of nutritional deficiencies (including fiber), poorly understood impact on the gut microbiom and the negative impact of long-term dietary restriction on mental health, it can’t be concluded that the ketogenic diet is completely safe. Of course, not every low-carbohydrate diet is a ketogenic diet. Maneuvering the proportions of consumed macronutrients can be used when designing nutritional strategies tailored to the individual needs and preferences of patients. Often, elimination diets also exclude multiple carbohydrate sources in order to determine whether these foods aggravate disease symptoms. An example of such a diet is the autoimmune protocol, which works great in the nutritional therapy of autoimmune diseases.
For now, I don’t see any reasons to follow the ketogenic diet in order to heal psoriasis, as better solutions exist. Maybe in the future new scientific evidence will emerge, but until then, I advise you to be cautious, especially if the ketogenic diet is going to be a long-term solution.
Bibliography
- Chalasani, S., Fischer, J. South Beach Diet associated ketoacidosis: a case report. J Med Case Reports 2, 45 (2008)
- Chen, T. Y., Smith, W., Rosenstock, J. L., & Lessnau, K. D. (2006). A life-threatening complication of Atkins diet. Lancet (London, England), 367(9514), 958.
- Blanco, J. C., Khatri, A., Kifayat, A., Cho, R., & Aronow, W. S. (2019). Starvation Ketoacidosis due to the Ketogenic Diet and Prolonged Fasting – A Possibly Dangerous Diet Trend. The American journal of case reports, 20, 1728–1731
- ng, Q. Y., Alexander, M., Newman, J. C., Tian, Y., Cai, J., Upadhyay, V., Turnbaugh, J. A., Verdin, E., Hall, K. D., Leibel, R. L., Ravussin, E., Rosenbaum, M., Patterson, A. D., & Turnbaugh, P. J. (2020). Ketogenic Diets Alter the Gut Microbiome Resulting in Decreased Intestinal Th17 Cells. Cell, 181(6), 1263–1275.e16.
- Henrick, B. M., Rodriguez, L., Lakshmikanth, T., Pou, C., Henckel, E., Arzoomand, A., Olin, A., Wang, J., Mikes, J., Tan, Z., Chen, Y., Ehrlich, A. M., Bernhardsson, A. K., Mugabo, C. H., Ambrosiani, Y., Gustafsson, A., Chew, S., Brown, H. K., Prambs, J., Bohlin, K., … Brodin, P. (2021). Bifidobacteria-mediated immune system imprinting early in life. Cell, 184(15), 3884–3898.e11.
- Groeger, D., O’Mahony, L., Murphy, E. F., Bourke, J. F., Dinan, T. G., Kiely, B., Shanahan, F., & Quigley, E. M. (2013). Bifidobacterium infantis 35624 modulates host inflammatory processes beyond the gut. Gut microbes, 4(4), 325–339.
- Georgescu, S. R., Tampa, M., Caruntu, C., Sarbu, M. I., Mitran, C. I., Mitran, M. I., Matei, C., Constantin, C., & Neagu, M. (2019). Advances in Understanding the Immunological Pathways in Psoriasis. International journal of molecular sciences, 20(3), 739.
- Coppola, S., Avagliano, C., Sacchi, A., Laneri, S., Calignano, A., Voto, L., Luzzetti, A., & Berni Canani, R. (2022). Potential Clinical Applications of the Postbiotic Butyrate in Human Skin Diseases. Molecules (Basel, Switzerland), 27(6), 1849.
- Desai, M. S., Seekatz, A. M., Koropatkin, N. M., Kamada, N., Hickey, C. A., Wolter, M., Pudlo, N. A., Kitamoto, S., Terrapon, N., Muller, A., Young, V. B., Henrissat, B., Wilmes, P., Stappenbeck, T. S., Núñez, G., & Martens, E. C. (2016). A Dietary Fiber-Deprived Gut Microbiota Degrades the Colonic Mucus Barrier and Enhances Pathogen Susceptibility. Cell, 167(5), 1339–1353.e21.
- Lindefeldt, M., Eng, A., Darban, H., Bjerkner, A., Zetterström, C. K., Allander, T., Andersson, B., Borenstein, E., Dahlin, M., & Prast-Nielsen, S. (2019). The ketogenic diet influences taxonomic and functional composition of the gut microbiota in children with severe epilepsy. NPJ biofilms and microbiomes, 5(1), 5.
- Paoli, A., Mancin, L., Bianco, A., Thomas, E., Mota, J. F., & Piccini, F. (2019). Ketogenic Diet and Microbiota: Friends or Enemies?. Genes, 10(7), 534.
- Kanda N, Hoashi T, Saeki H. Nutrition and Psoriasis. Int J Mol Sci. 2020 Jul 29;21(15):5405.
- Castaldo, G., Rastrelli, L., Galdo, G., Molettieri, P., Rotondi Aufiero, F., & Cereda, E. (2020). Aggressive weight-loss program with a ketogenic induction phase for the treatment of chronic plaque psoriasis: A proof-of-concept, single-arm, open-label clinical trial. Nutrition (Burbank, Los Angeles County, Calif.), 74, 110757.
- Castaldo, G., Galdo, G., Rotondi Aufiero, F., & Cereda, E. (2016). Very low-calorie ketogenic diet may allow restoring response to systemic therapy in relapsing plaque psoriasis. Obesity research & clinical practice, 10(3), 348–352.
- Castaldo, G., Pagano, I., Grimaldi, M., Marino, C., Molettieri, P., Santoro, A., Stillitano, I., Romano, R., Montoro, P., D’Ursi, A. M., & Rastrelli, L. (2021). Effect of Very-Low-Calorie Ketogenic Diet on Psoriasis Patients: A Nuclear Magnetic Resonance-Based Metabolomic Study. Journal of proteome research, 20(3), 1509–1521.
- Crum, A. J., Corbin, W. R., Brownell, K. D., & Salovey, P. (2011). Mind over milkshakes: mindsets, not just nutrients, determine ghrelin response. Health psychology : official journal of the Division of Health Psychology, American Psychological Association, 30(4), 424–431.